Extraordinary Academic Programmes with Outstanding Values
We Speak Science places a strong emphasis on work experience. We give students the opportunity to work one-on-one with a leading academic from a world-class institution who will guide, mentor, and provide students with the invaluable academic knowledge and key professional and life skills they need to succeed and lead through uncertainty in the 21st century.
Our science courses offer students an opportunity to learn from world-leading experts from Ivy League institutions and organisations, including Harvard University, the University of Oxford, and NASA scientists.
Residential Courses
Join us in the We Speak Science Summer programmes for an unforgettable educational experience based at University of Oxford, the University of Cambridge, the University of Harvard, or MIT. The program will be taught by world-class academics.
If you would like to know more information about our Residential programmes, please contact:
info@wespeakscience.com
Online Programmes
Gain extensive knowledge of a subject of your choice. Learn from world renowned academics from the University of Oxford, the University of Cambridge, the University of Harvard, MIT, or other Ivy League Universities. Study alongside other students from around the world, one-to-one or in small group settings. Available to students globally.
WSS alumni
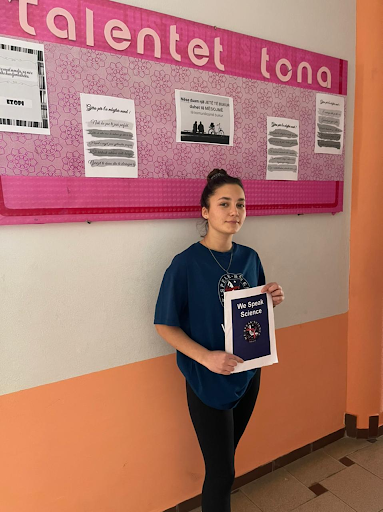
share their stories
Hear from some previous participants who took part in the We Speak Science programme.
Alvsia A
Attended WSS in 2021
I chose to enroll in the We Speak Science Online STEM course to explore data science and biomedical science in depth. I found it challenging to prepare a presentation and analyze scientific data, but it was very rewarding. I enjoyed learning about research methods in biochemistry and analyzing scientific research data carried out in space. I really enjoyed learning about data science and I want to continue studying it.
Academic Insights participant

Enisa A
Attended WSS in 2021
I took the Future Scientist Course on the We Speak Science Online Programme. I am a very shy person, and I thought that I would have a problem communicating with my supervisors, but as soon as we started our first lesson, all my nerves went away, and I started talking normally as if I was talking to a friend!
I found the course really useful to better understand what business is. Now that I have tried it out, I would love to continue studying it.
Research Scientist Course

Jessica M
Attended WSS in 2021
We Speak Science gave me confidence and taught me about leadership and teamwork. It taught me to be independent, not be afraid to try new things (even if they don’t work), and believe in myself. I will never forget this experience because it has inspired me to dream big. Thanks to We Speak Science, I am inspired to study at Harvard or MIT. I will apply to study at both universities, and then wait for the outcome, hoping that I will get in.
Attended We Speak Science 2021

Florentina A.
Attended WSS in 2021
Thanks to the We Speak Science, I am now the lead UI/UX designer for an outstanding company that creates AI apps. Taking the STEM course in We Speak Science was fundamental to my success. I learned about AI and data science and engaged with world-leading experts from whom I learned a lot. The We Speak Science STEM course was very dynamic and interactive. I felt engaged and immersed in the AI field. The programme was flexible, and I could have followed it remotely from anywhere. I was able to work and study at the same time.
Attended WSS STEM Course in 2021

Era A
Working as a full-stack software developer in Germany, I am always looking for the next step. My dream job and passion are to somehow combine computer science with medicine. We Speak Science academy was the perfect place for me to start that journey. The amazing courses from such experts not only teach me a lot, but also keep me motivated, engaged, and thirsty for learning more and more.
Academic Insights participant




Meet our
World-class experts
An extraordinary educational experience taught by world-class STEM experts where students are at the center of our programmes.
